More than just a skin disorder
Psoriasis is not just a cosmetic problem: Even patients with mild symptoms are impaired in their daily activities.
Due to the physical appearance of psoriasis, this disease often leads to psychological problems, such as depression and marginalisation. Even people with mild expression of the dermatological symptoms feel compromised in their daily activities. The limitation to the quality of life may be particularly serious, if the disease is very obvious, as on the face, for instance.
Symptoms and co-morbidities
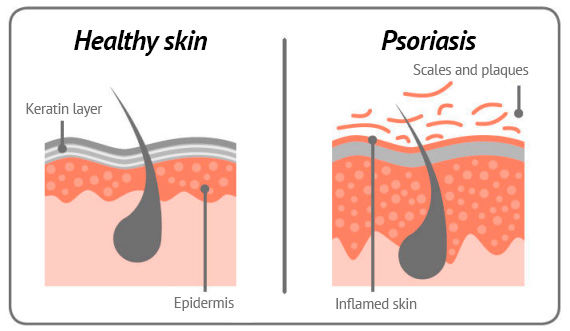
The most commonly affect skin regions include elbow and knee joints, and head or nails areas. The affected patches are covered with silvery-whitish scales.
Patients with psoriasis more commonly suffer from metabolic disorders, such as type II diabetes. Moreover, there is a higher risk of cardiovascular diseases in these patients. These patients are more commonly overweight and depressed than healthy people.
Psoriasis is not just a skin disease.
Up to 30% of people suffering from psoriasis also develop psoriatic arthritis
About a quarter of the patients with skin symptoms may develop an inflammatory joint disease, which can cause pain, stiffness and swelling.
What causes psoriasis?
We do not yet know exactly what causes psoriasis. A combination of genetic predisposition and environmental factors may trigger the disease or cause it to flare up. It is not predictable if and when psoriasis will develop.
Infections, medications, obesity and nicotine consumption are environmental factors that may contribute to a worsening of the psoriasis. The effects of stress cannot be underestimated: Family problems or professional stress have a negative effect on the development of psoriasis.
We differentiate between different types of psoriasis:
- Plaque Psoriasis (common psoriasis): This is the most common type of psoriasis. The red, silvery scales may show up on the entire surface of the body. The name "Plaque psoriasis" is derived from these changes – the plaques. Some patients also suffer from psoriasis of the finger and toe nails (psoriatic nail disease). This is characterised by small dents (pitted nails), discolourations (oil stains) and separation of the nail plate.
- Guttate psoriasis: This often very itchy type commonly appears after infections and appears as a large number of small, dot-like lesions ("guttate" means dot-like).Pustular psoriasis: In this rare type, white pus-filled blisters form on red skin patches. It may affect individual patches only (for example the palms of hands and soles of feet), or the entire surface of the body.
- Psoriatic nail disease: Nail changes may develop in all types of psoriasis. The finger nails are affected in around half of patients, and the toe nails to a slightly lesser extent
Psoriatic arthritis
Psoriatic arthritis is – like psoriasis – a chronic, progressive immune disease. Psoriatic arthritis can lead to painful inflammation of joints, spine, tendon insertions, tendon sheaths or bursae.
About 30% of people with psoriasis are affected by this inflammatory rheumatic disease. Although psoriatic arthritis is a combination of psoriasis and inflammatory rheumatism, joint and skin infestation need not occur simultaneously. In about 80%, the skin and nail changes occur before the changes in the joints.
Typical symptoms of psoriatic arthritis include morning stiffness, pain at rest and swelling. The small joints on the hands, knees or ankles are often affected. The spine often hurts at the neck and coccyx, and in the case of tenosynovitis, there is prominent inflammation of the Achilles tendon. Psoriatic arthritis is typically characterised by the mostly asymmetrical involvement of often less than five joints.
The cause of psoriatic arthritis is not known, although genetic predisposition and environmental factors may play a role. According to current knowledge, psoriatic arthritis is not curable and can lead to irreparable joint damage. Timely diagnosis by a rheumatologist is therefore important. It is therefore recommended that people with psoriasis inform their doctors of any joint pain.
With an individually tailored therapy, skin and joint symptoms can be largely controlled, and deterioration of the joints prevented. In addition, non-pharmaceutical therapies can positively support the treatment, such as physiotherapeutic treatments, lifestyle adjustments and targeted body and mobility training.
